
Pandemic Lesson: Health Care Systems Need Significant Investment Starting at the Primary Level
Key Messages
- A high quality primary health care (PHC) service will reduce inequities; increase labour market participation; reduce costs; save foreign exchange; improve public health systems; and, ultimately, save lives in the Caribbean.
- Mitigating public health crises such as the COVID-19 pandemic and achieving sustainable universal health coverage (UHC) require significant investment in primary health care (PHC) services.
- Sustainable and affordable universal health coverage necessitates a regional approach, in material aspects, such as governance; the creation of a digital health ecosystem; and the procurement of personal protective equipment (PPE) and other medical supplies and equipment.
Introduction
One of the enduring lessons of this pandemic is the criticality of investment in our health systems, especially primary health care. The emergence of the Novel Coronavirus-2019 in late 2019 has led to the biggest global public health crisis in our lifetime – the COVID-19 pandemic. As at July 02, 2021, the virus has infected over 182.0 million people globally and led to almost 4.0 million deaths in 235 countries. The most recent data show that COVID-19 infections in the Eastern Caribbean Currency Union (ECCU) have increased to over 9,700 confirmed cases, with 143 deaths. Many of these deaths appear to be linked to co-morbidities, that is, the incidence of chronic diseases such as diabetes, hypertension and heart disease among persons infected by COVID-19. Never forget, according to a report published in 2020 by the Caribbean Public Health Agency (CARPHA), in 2016, almost 8 out of every 10 deaths in the Caribbean were due to non-communicable diseases (NCDs), a pre-pandemic epidemic in our region.
report published in 2020 by the Caribbean Public Health Agency (CARPHA)
Many health systems in countries large and small were simply unprepared for a public health crisis of this magnitude. Relatively speaking, as the data show, the ECCB member governments have managed the pandemic well. This pandemic occurred at a time when some ECCB member countries were making strides towards achieving Universal Health Coverage (UHC) and, in particular, had turned their focus towards the implementation of National Health Insurance (NHI), a key policy objective. It cannot be overstated that a strong health care system is essential to developing a healthy population and, ultimately, to building a resilient people and economy.
The United Nations General Assembly in its Sustainable Development Goals (UNSDG) agreed to Universal Health Coverage in 2015 (UNSDG 3.8). However, achieving UHC and mitigating public health crises require significant primary health care investment. Primary Health Care (PHC) covers a range of care services including health promotion, prevention and treatment of diseases, rehabilitation and palliative care. Through PHC, countries are able to provide holistic care to communities and, in so doing, achieve greater resilience in the health care sector and the economy.
Key challenges for the region, such as NCDs and infectious disease outbreaks, can also be addressed and or mitigated through a robust PHC service. PHC is based on three key pillars: (i) community empowerment; (ii) multi-sector policies and policy implementation; and (iii) delivery of primary care and public health services of substantial quality (Ghebreyesus et al., 2018).
The continuous design of health systems around these three pillars will lead to better health outcomes in ECCB member countries both from a public health perspective as well as a broader macroeconomic perspective. Indeed, the successful implementation of high quality primary health care services can deliver the following benefits:
- Equitable access and slower growth in health care spending;
- Labour market improvements, including increased labour market participation and productivity;
- Improved fiscal sustainability;
- Robust and emergency-ready health systems; and
- Reduced rates of non-communicable diseases, HIV/AIDS, maternal and infant mortality and multimorbidity.[1]
Access to health care services is a key indicator for gauging the extent of primary health coverage as well as progress towards Universal Health Coverage. The World Health Organization (WHO) Health Access Index of selected ECCU member countries shows that access to health care systems varies within the region, with service and access being highest in Antigua and Barbuda (Figure 1).

World Health Organization (WHO) Health Access Index
Additionally, ensuring the reduction of gaps in access to primary care services is key to achieving full health service coverage. Consequently, member countries should continue to scale up primary health care (essential) services, whilst making efforts to reduce the costs borne by their citizens who cannot afford to pay. ECCB member governments can also enhance the delivery of Primary Health Care services through continued investment in health care service providers, however, they must return and give back to their countries of birth and sponsorship. A sufficiency of these providers is necessary to aid in the delivery of PHC services. These health care providers include physicians, nurse practitioners, nurses and dentists[2]. Data from the Pan American Health Organization (PAHO) show that only three (3) ECCB member countries have a total workforce of nurses per 10,000 that is greater than the regional average of 35.5. For physicians, only two (2) ECCB member countries have a workforce of physicians that is greater than the regional average of 24.1, while no ECCB member country has a workforce of dentists that is greater than the regional average of 4.0 (Figure 2).

The cost of access to PHC services also remains a challenge for ECCB member countries. The most recent data provided by the WHO show that, at the end of 2016, the average cost of care per capita for citizens in ECCU member countries was approximately US$260.48, whilst estimates are that ECCU member governments spent approximately US$241.54 per capita. Thus, the burden of the cost of care between citizens and member governments is approximately 50:50. Evidently, this burden of cost, means that some citizens find access to health care to be financially prohibitive. This cost sharing between governments and citizens is a necessary though not sufficient condition for the establishment of a robust NHI in the ECCU and, consequently, a reduction in the cost of services for member countries (Cumberbatch, 2020). Moreover, with a high cost of care, low or uneven access to and low investment in PHC services, public health crises such as the COVID-19 pandemic are likely to exacerbate other inequities that may exist in health care systems, including those related to gender and other marginalized groups within society (Cataldo, 2020).
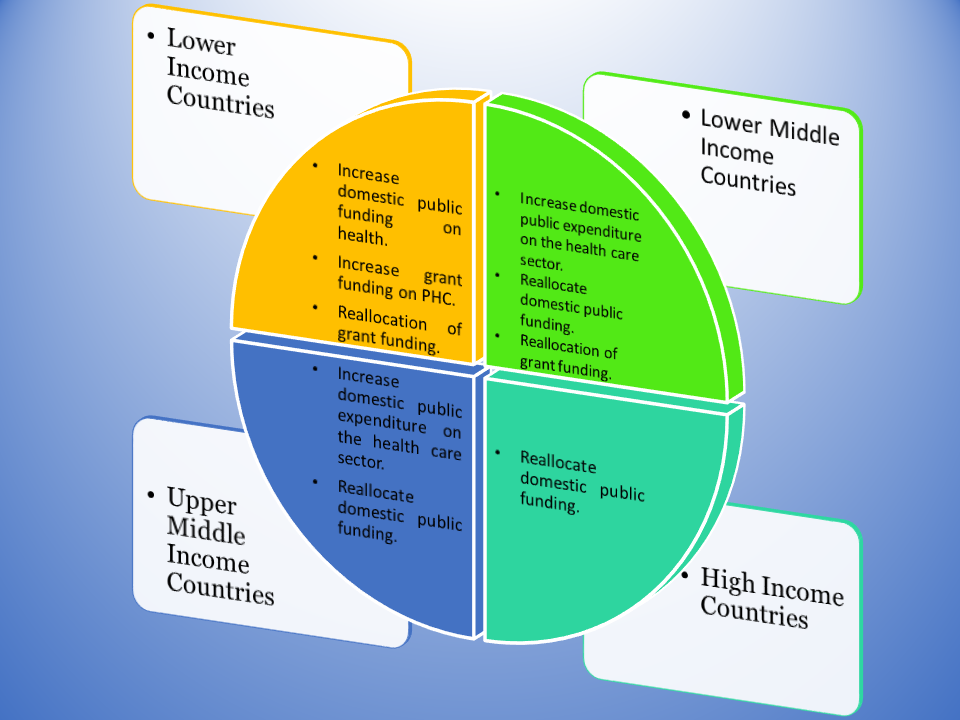
The current level of expenditure on health care services could also assist ECCU member governments in achieving additional coverage through the PHC. For some ECCB member countries, achieving increased investment in PHC services may require different approaches (Figure 3). ECCB member countries with limited fiscal space can examine other approaches listed below and more suited to their macroeconomic context. These approaches can create fiscal space for increased investment in infrastructure, equipment and beds. Furthermore, existing mechanisms such as the Organisation of Eastern Caribbean States Pharmaceutical Procurement Service (OECS PPS) is highly suited for the procurement of the aforementioned equipment, especially in national emergencies.
Call to Action
In light of the foregoing, what can ECCB member countries do to enhance PHC services?
- Establish a digital health ecosystem which can reduce gaps in PHC services and allow for higher quality care, scalability and cost reduction.
- Examine current efforts geared towards the implementation of a National Health Insurance and take stock of lessons in countries such as British Virgin Islands and Cayman Islands to ensure a sustainable approach to this key policy objective. This is essential to, in time, reduce the cost burden for ECCU citizens and residents while providing greater access to PHC services.
- Establish minimum standards of care and specialization centres across the ECCB member countries. Health care is very expensive. The idea of individual countries trying to go it alone is neither feasible nor sustainable.
- Expand the use of the OECS Pharmaceutical Service. The OECS Commission, to its credit, has recently invested in a platform that allows more aggressive bidding and auctions thereby securing lower prices and better value for member countries. It is estimated that countries pay about 20 per cent less for products procured through this Service than they would otherwise pay.
Given the myriad health challenges of our region and the very limited fiscal space of our governments, a coordinated approach to PHC services is critical. Such an approach, premised on the foregoing considerations, would provide a stepping-stone to offer more robust primary health care to ECCU citizens and residents, whilst achieving Universal Health Coverage and an integrated National Health Insurance system – a hitherto elusive aspiration for ECCB member countries.
Our relentless pursuit of resilience continues.
- Multimorbidity refers to, “the coexistence of two or more chronic conditions in the same individual.”
- Data for dentists in Antigua and Barbuda is absent from this health worker density chart.
Acknowledgement
The ECCB acknowledges the contribution of Mr Shernnel Thompson, Deputy Director (Ag.), Research Department, in the preparation of content for this blog.
About the Author
Timothy N.J. Antoine has been the Governor of the ECCB since February 2016. He is passionate about the socio-economic transformation of the Eastern Caribbean Currency Union (ECCU) and is a strong advocate for regional cooperation and collective action. Indeed, he regards them as critical to shared prosperity for the people of the ECCU.
About the Eastern Caribbean Central Bank
The Eastern Caribbean Central Bank (ECCB) was established in October 1983. The ECCB is the Monetary Authority for: Anguilla, Antigua and Barbuda, Commonwealth of Dominica, Grenada, Montserrat, Saint Christopher (St Kitts) and Nevis, Saint Lucia and Saint Vincent and the Grenadines.


